Does diet affect migraines?
Reviewed by Dr Bhavini Shah
In this article, we will explore the link between diet and migraines, including migraine food triggers, and the foods which may potentially help reduce their impact. And to find out more, we surveyed* 500 Brits to explore the link between diet and migraines, including food and lifestyle triggers, and the ways which may potentially help to reduce their impact.
What are migraines?
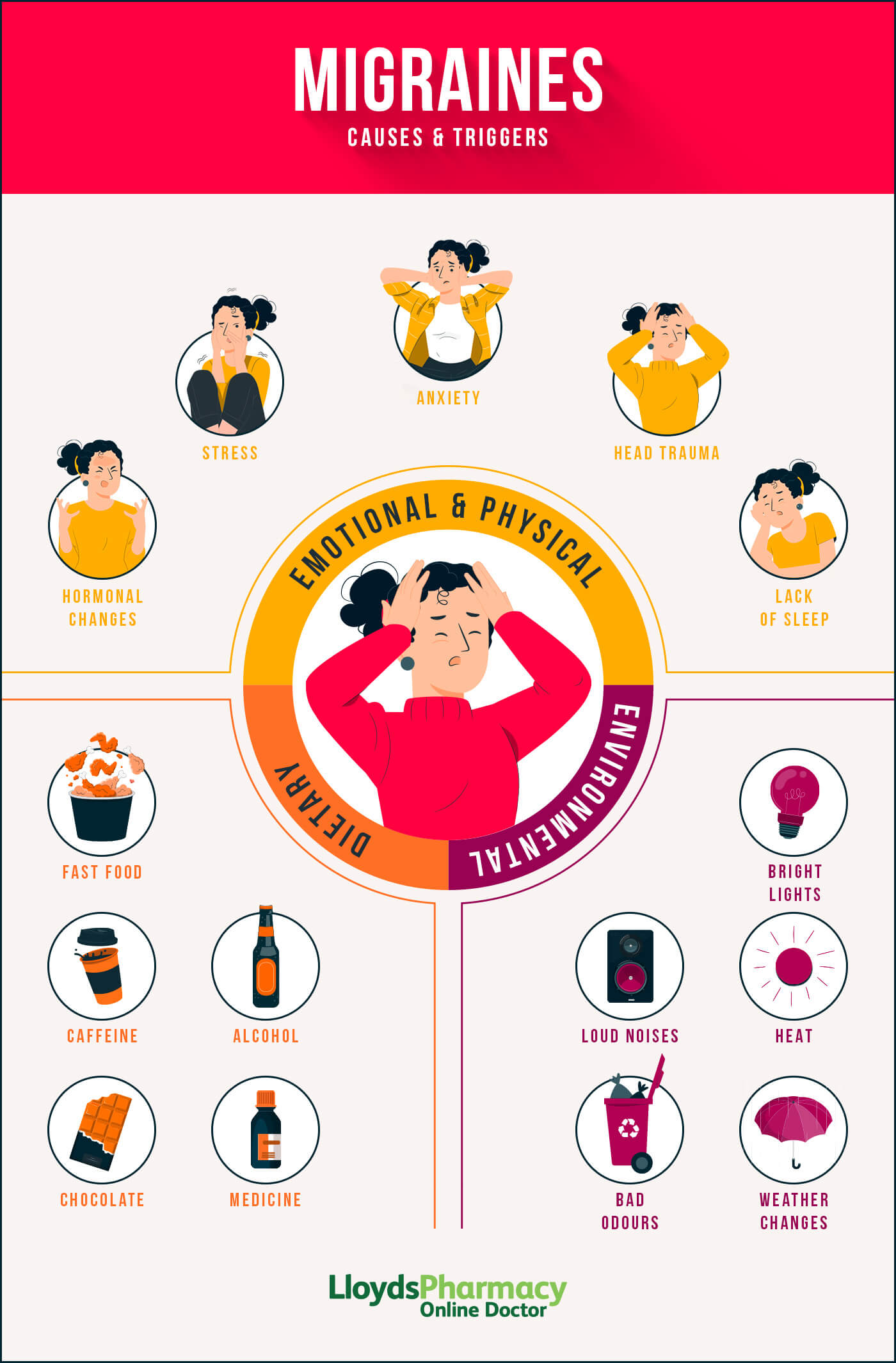
Migraines are a type of headache that typically causes recurring, one sided headaches that can last up to 72 hours. It’s thought that around 10 million people experience migraines in the UK every year. They can be triggered by stress, noise, certain smells, alcohol, lack of sleep, or dehydration. Research suggests that diet may also play a significant role.
The exact cause of migraines is unknown, although can be triggered by a number of factors, from hormonal changes and certain foods or drinks, to stress and environmental factors. They can also be triggered by changes in sleep patterns or weather.
They are often accompanied by other symptoms such as sensitivity to light, sound, or smell, nausea and vomiting, and can occasionally be associated with visual disturbances such as seeing spots or flashes of light.
What foods and drinks trigger migraines?
“Certain foods and drinks have been identified as potential triggers for migraines,” explains Dr Bhavini Shah, “either in scientific studies or anecdotally by people who experience them”.
Here are some of the most noted migraine food triggers:
Caffeine
Caffeine has long been part of the treatment of migraines, and for some people a withdrawal of caffeine triggers migraines rather than drinking coffee. However, some people find that they cannot drink coffee once their migraine has started. 31% of respondents attributed caffeine as a cause of their migraines, but only 6.4% have actually cut down their intake to help alleviate their symptoms.
Alcohol
Alcohol can also be a trigger for migraines. Alcohol works in the opposite way to caffeine, causing the blood vessels in the brain to expand, leading to headaches. Additionally, alcohol can also disrupt sleep patterns, which might also trigger migraines.
One in three revealed that alcohol was a trigger for their migraines, with 33% of those holding prosecco responsible. This was followed by champagne at 31%, beer and ciders at 28% and 25%, while a quarter of Brits say tequila triggers their migraines.
Wine causes in 27% of our survey respondents. Red wine is particularly associated with migraines, this is because it contains a chemical called tyramine. Tyramine is known to dilate blood vessels, potentially causing headaches or migraines.
Sweeteners
Artificial sweeteners, such as aspartame, might be potential triggers for migraines. And this was the case for almost one in 10 respondents. These can be found as a substitute for sugar in a variety of diet products or sugar-free drinks, so if you find sweeteners to be a potential trigger it might be best to switch out soft drinks with sweeteners to water instead.
Interestingly, 89% of those surveyed didn't know that artificial sweeteners could be a potential cause of migraines.
MSG (Monosodium glutamate)
MSG, a common food additive, is sometimes reported as triggering migraines. You find MSG in some processed foods and it’s often in Chinese cooking. However, according to our survey, 94% of respondents were unaware of correlation between MSG and their migraines.
Cured meats
Cured meats, such as bacon and deli meats, are sometimes reported as a trigger for migraines. They contain nitrates, which dilate blood vessels and could potentially lead to headaches or migraines. From our study, less than 1% were aware that cured meats are a trigger for migraines, which is something to keep in mind if you do suffer from symptoms.
Dairy
Dairy products, particularly soft cheese like brie and camembert, are reported by some to be a trigger for migraines as they also contain tyramine.
Despite being a common trigger, only 4.6% respondents were aware that cheese can cause migraines.
Pickled or fermented food
Fermented or pickled foods, such as pickles, sauerkraut, and soy sauce, are sometimes reported by people experiencing migraines as triggers. These types of foods, much like red wine and soft cheeses, often contain high levels of tyramine.
Salty foods
Salty foods might also be a trigger for migraines. High salt intake can lead to dehydration, which can cause headaches. Lowering your salt intake and increasing your water intake can lessen the negative effects of dehydration.
Chocolate
Some people do say that chocolate causes their migraines. However, it's thought that lots of people crave chocolate/sweet things as a migraine is oncoming, and that's why they might think eating it is the trigger.
What foods and drinks help migraines?
Just as certain foods can trigger migraines, there are also foods and food habits that might help to prevent or reduce the frequency and severity of migraines. Here are a few examples:
Leafy greens
Leafy greens, such as spinach and kale, are rich in magnesium. Magnesium is a natural muscle relaxant and might help to reduce the frequency and severity of migraines.
Omega-3 fatty acids
Foods that are high in omega-3 fatty acids, such as fatty fish, flaxseed and chia seeds, can help to inhibit the production of chemicals which cause inflammation, potentially preventing migraines.
Water
Staying hydrated is important for your overall health, and it can also help to prevent migraines. Dehydration can cause blood vessels to constrict, which can lead to headaches. You should drink at least 8 glasses of water a day to stay hydrated. When it comes to migraines, more than one in four survey respondents agreed that dehydration was a leading trigger for them.
It's important to keep in mind that a balanced diet includes a variety of fruits, vegetables, whole grains and lean proteins, and you should make sure you’re getting all the nutrients you need. A food diary will help you identify triggers while still ensuring you eat a healthy, balanced diet. A doctor or a dietitian can then help you create a personalised migraine diet plan.
What is the best migraine diet?
When it comes to migraines, there isn't a one-size-fits-all diet solution. However, changing your diet could potentially make a big difference to your migraines. Apart from having a healthy balanced diet avoiding processed and ultra processed foods you could try the following:
High folate diet
Folate deficiency may lead to physical symptoms including migraines, so having a diet that's rich in leafy greens and fresh fruit is a way of preventing this.
Low-fat diet
Eating a diet that is low in fat may help to prevent migraines. The relationship between a low-fat diet and fewer migraines is not well understood, but it does seem to work for some people.
High omega-3
Omega-3 fatty acids can help to reduce inflammation and may prevent migraines. Eating foods that are high in omega-3 fatty acids, such as fatty fish, flaxseed and chia seeds, might help to reduce the frequency and severity of your migraines.
Low sodium diet
There has been some research into sodium (salt) levels and migraines, and it seems that a low sodium diet can help with reducing migraine episodes - apart from reducing cardiovascular risks.
What else can trigger a migraine?
Migraine triggers are different for everyone, and what triggers migraines in one person might not trigger them in someone else. However, some common shared triggers have been documented:
Hormonal changes
Hormonal changes, particularly those that occur during the menstrual cycle, can trigger migraines in some women. More than half of the women who experience migraines find that there is a link to their period.
From our survey, 85% were unaware that hormone changes have any impact on migraines. However, for those who are affected tracking your symptoms alongside your menstrual cycle could be beneficial to determining the trigger
Stress
Stress is a well-documented trigger for migraines. It is thought that stress affects hormones and neurotransmitters (chemicals) that modulate and regulate the perception of pain. Serotonin is one of these neurotransmitters.
More than one in 10 respondents revealed work stress as a leading trigger for their migraines, with the highest number coming from those working in law enforcement.
Environmental triggers
Certain environmental triggers, such as changes in weather, bright lights, or strong smells, can also trigger migraines in some people, although we don’t really understand why. Atmospheric pressure changes (usually a decrease in barometric pressure) can trigger migraines in some people.
Sleep patterns
Poor sleep hygiene - either getting too little or too much sleep - can also be a trigger for migraines. More than one in 10 survey respondents said that irregular sleeping patterns were a leading trigger for their migraines, while 20% find getting more sleep is a natural remedy for their migraines.
Physical triggers
Certain physical triggers, such as neck or head trauma, can also trigger migraines.
It's important to note that everyone's triggers are unique and it may take some time and experimentation to identify yours. Keeping a headache diary is a good first step to identifying triggers. There are several apps that can help you do this; if you prefer a paper version you can download a diary from the migraine trust. Once you have identified your triggers, you can take steps to avoid them, which can help reduce the frequency and severity of your migraines.
It's also worth mentioning that, sometimes, even when avoiding triggers, migraines may still occur. This is because migraines can also be caused by genetic and neurological factors that cannot be controlled. That’s why it’s also important to have a plan for managing migraines when they do occur, such as taking medications or using relaxation techniques.
How to find out your personal migraine triggers
A good headache and food diary (manual or app based) can help you identify food triggers. Triggers tend to be different from person to person, so it's impossible to make general recommendations. A headache diary/app might also help you to identify other triggers such as sleep, weather or general stress issues.
Once you have a better idea of what might be triggering your migraines, you can then start to tackle it. If your triggers are food or drink based, you can gradually restrict your diet to eliminate them. You should only ever make big changes to your diet under the supervision of a doctor or dietician, to make sure you’re still getting everything you need.
How to treat migraines
Migraines can be debilitating and severely impact your day to day life, but there are ways to treat them and minimise the effect they have. Treatment should involve a combination of measures, such as medication and lifestyle changes. Your approach will vary depending on the severity and frequency of your migraines, as well as any underlying health conditions that may be causing your symptoms.
According to Dr Neel Patel, GP:
"While the triggers for migraines can vary widely from person to person, it may take some trial and error to determine which foods are responsible, especially if you aren’t aware of the foods and drinks that could be problematic for you."
"We recommend keeping a food diary which can help you to identify patterns and triggers for your migraines. If you suspect that certain foods are leading to symptoms, try eliminating them from your diet for a while to see if they improve."
Here are a few methods to consider:
Medications
There are several types of medications that can be used to treat migraines, including over-the-counter pain relievers, triptans, Vydura (rimegepant), certain antidepressants and even certain blood pressure tablets. These medications can help reduce the pain and symptoms of migraines. You should speak with a doctor to determine which medication is best for you.
Non-medication therapies
Non-pharmacological therapies such as biofeedback, acupuncture, and cognitive behavioural therapy (CBT), might also help to reduce the frequency and severity of migraines, although there is still a lack of evidence to support many holistic claims. CBT is highly effective at reducing stress and anxiety, which may in turn reduce the severity and duration of migraines due to tension.
Certain supplements, such as magnesium and riboflavin have been shown in studies to reduce the frequency and severity of migraines, however there needs to be more research into this area.
Preventive measures
Preventive measures such as regular exercise, stress management, and maintaining a consistent sleep schedule can all help to reduce migraines. Avoiding known triggers and eating a healthy diet can help. Keeping a migraine diary can help you to track when your migraines occur, how long they last, what triggers them, and what helps relieve them. This can also help you to identify patterns and avoid triggers that may aggravate them in the future.
Self-care techniques
Self-care techniques such as relaxing in a dark room, applying a cold compress to the head, and massaging the temples can reduce the pain and discomfort during a migraine.
If stress is a common trigger for your migraines, practicing relaxation techniques such as deep breathing or meditation can be helpful in managing stress-related migraines. Getting regular exercise can also help to reduce the frequency and severity of migraines as well as maintain a regular sleep schedule.
Conclusion
Migraines can potentially be triggered by diet, so if you regularly experience migraines, this might be a good place to start. Changing your diet may help reduce the frequency and severity of migraines days. Eating more leafy greens, including foods high in omega 3 fatty acids and magnesium, staying well hydrated and avoiding highly processed foods would be a good place to start.
Identifying personal migraine triggers by keeping a diary and noting symptoms after eating certain foods can also help in managing migraines. It is important to consult with a doctor or healthcare professional, to confirm the diagnosis.
Remember that everyone experiences migraines differently and what works for one person may not work for another. It’s important to be patient and persistent as you work to find the best treatment for you.
Always speak with your healthcare provider before making any significant changes to your diet or trying a home treatment plan.
*Methodology
Onepulse conducted a survey on behalf of Lloyds Pharmacy Online Doctor and surveyed 500 male and female respondents in the UK between 16/03/23 and 17/03/23. They were then given three questions of multiple choice to describe their experience with migraines in relation to a number of different factors.
References
https://www.england.nhs.uk/2020/01/improved-nhs-migraine-care/
https://www.nhs.uk/conditions/hormone-headaches/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7468766/
https://migrainetrust.org/news/chocolate-and-migraine
https://migrainetrust.org/live-with-migraine/self-management/common-triggers/
https://pubchem.ncbi.nlm.nih.gov/compound/Tyramine#section=Absorption-Distribution-and-Excretion
https://www.ajmc.com/view/review-outlines-relationship-between-magnesium-deficiency-migraine
https://pubmed.ncbi.nlm.nih.gov/10839648/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8628940/





