Cluster headaches vs. migraine
Reviewed by our clinical team
When talking about severe headaches, the impact they can have, and the treatments available, distinguishing between cluster headaches and migraines is crucial.
Although both conditions present with debilitating head pain and can significantly impact quality of life, they’re fundamentally different, and identifying which you’re experiencing is a vital part of finding the right treatment.
In this article, we’ll take a look at the symptoms of both cluster headaches and migraines, explore the potential triggers, and discuss the available treatment options and strategies to help you find the best course of action.
What is the difference between migraine and cluster headache?
Migraines are a debilitating condition which usually present with moderate to severe headaches, often accompanied by nausea and sensitivity to light and sound, known as aura.
Migraines might happen once or be a recurring (chronic) issue, with attacks lasting from a few hours to several days. These chronic migraines can cause significant disruption to everyday life, making even simple tasks such as phone calls or watching television impossible.
Cluster headaches, in contrast, are generally shorter, lasting just minutes to hours, but are more acutely intense and painful, and tend to recur more frequently, usually over several weeks or months in what are known as clusters.
While migraines linger, causing extensive discomfort, cluster headaches are intense but transient, usually marked by a piercing pain on one side of the head. This pain is often so unbearable that cluster headaches have been described as ‘suicide headaches’.
Understanding these contrasting symptoms is crucial for effective headache management and treatment. Read our guide for more detailed insights on the differences between migraines and headaches.
What is a cluster headache?
Cluster headaches are incredibly painful headaches that occur in patterns or ‘clusters’, typically experienced on one side of the head, around or above the eye. These headaches are known for their sudden onset and can present with a sharp, piercing, or burning pain.
Cluster headaches can often be so severe and debilitating that they might prevent individuals from performing even the simplest daily tasks.
Cluster periods can last for weeks or even months. During these periods, individuals may experience headaches at the same time each day, with each attack lasting between 15 minutes to 3 hours.
Cluster headaches are also known for their remission periods, where the headaches stop entirely for months or even years before reoccurring. These remission periods can offer significant relief and a return to normal life, but also mean that people who experience cluster headaches often spend their lives in fear of the next flare-up.
Knowing what a cluster headache is and how it presents makes it easier to find the appropriate treatment and mitigate the impact of these painful episodes.
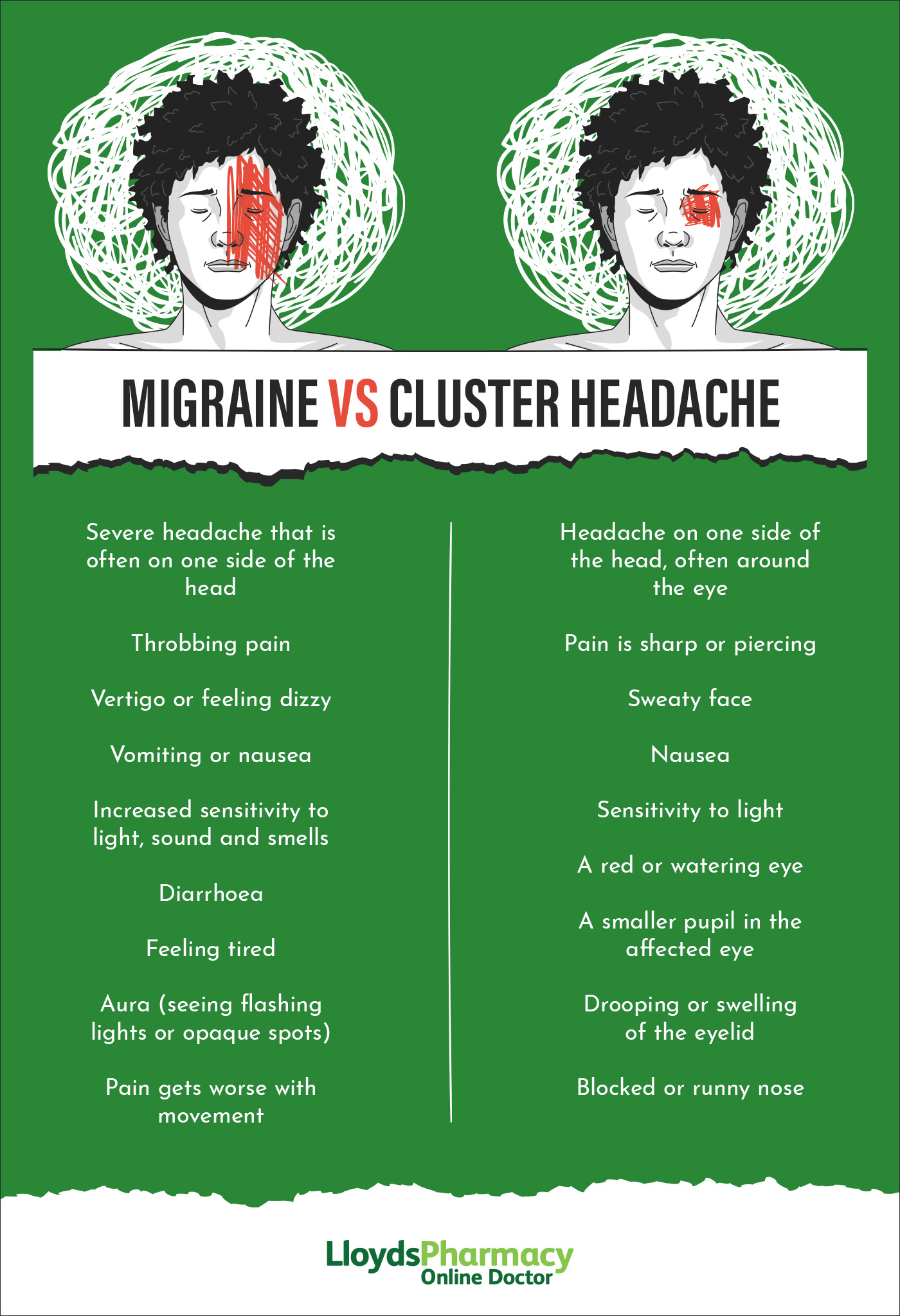
Migraine vs. cluster headache symptoms
Migraines and cluster headaches are often mistaken for one another, but they’re actually quite different. Migraines can cause pain in varying locations, including on the sides of the head, behind the eye, in the back or the front of the head, or throughout the entire head. Conversely, cluster headaches almost always occur on one side of the head, usually around the temple or eye.
People with migraines often find that dark and quiet rooms can bring relief, while those dealing with cluster headaches struggle to find any relief at all. They might also display signs of agitation or overstimulation.
Although they share symptoms beyond head pain, such as eye redness, tears, and nasal congestion, these are again typically on both sides of the head with migraines and only one side with cluster headaches.
Migraines also generally present with nausea and vomiting, which aren’t typically associated with cluster headaches.
Keeping track of your symptoms with a headache relief diary is an effective way of identifying whether you’re dealing with a cluster headache or migraine, helping you find the right treatment.
How long do cluster headaches last?
Migraines generally last much longer than cluster headaches - potentially several days - while a cluster headache typically lasts no longer than three hours, but is more intense and acutely painful.
Although cluster headaches have a notably shorter duration compared to migraines, what makes them particularly distressing is the frequency at which they can occur during a cluster period, and the length of time these cluster periods can last.
There are two types of cluster headache, episodic and chronic. Episodic cluster headaches manifest in bouts that last from seven days to one year, interspersed with pain-free intervals usually lasting at least three months. Chronic cluster headaches, meanwhile, generally present with sustained attacks for over a year without any remission, or with remission phases lasting less than three months.
It’s thought that around 2 in 10 individuals with cluster headaches experience the chronic type.
A person experiencing cluster headaches might endure up eight cluster headaches in a single day, interspersed with pain-free intervals. Although these headaches are transient, their regularity and intensity can significantly impact daily life.
Identifying whether you’re dealing with a migraine or a cluster headache can be challenging due to the overlapping symptoms, but by tracking the duration of the headache and accompanying symptoms closely, getting the correct diagnosis can be much more straightforward.
Cluster headache causes
As with migraines, the exact cause of cluster headaches remain largely unclear, and much of what we know about them is derived from anecdotal evidence and personal reports.
Some doctors believe that abnormalities in the hypothalamus, which is responsible for crucial bodily functions such as regulating temperature, thirst, sleep, blood pressure, and heart rate, could play a role. There might also be a genetic component, as those experiencing cluster headaches often report a family history.
Although stress is often reported as a migraine trigger, there’s no evidence to suggest it plays a role in cluster headaches as yet.
Additionally, alcohol consumption and smoking could be potential triggers or worsening factors, especially during cluster period. To explore possible triggers and management strategies for headaches, check out our article on avoiding the most common migraine triggers.
How common are cluster headaches?
Despite their severe and debilitating nature, cluster headaches are relatively rare, afflicting approximately one in 1,000, or roughly 65,000 people in the UK. Cluster headaches generally begin after the age of 30, and predominantly affect males, with a ratio of around 6:1.
This unfortunately makes researching the condition more difficult, another reason why it is important for those experiencing cluster headaches to track their episodes, the symptoms which come with them, and talk to their doctor.
Treating migraine vs. cluster headache
When seeking help for cluster headaches it’s important to recognise that, although they share some common symptoms with migraines, the treatments for the two conditions vary. While migraines have a broader range of treatments, including over-the-counter medications, the severe and specific nature of cluster headaches often requires specialised treatments.
Migraine treatment
- A type of medicine known as triptans are often very effective for more severe migraines, and are available in various forms including tablets, nasal sprays, and injections. Sumatriptan and rizatriptan are two of the most commonly prescribed migraine treatments in the UK, and are both available through our online service.
- Lifestyle changes, such as losing weight, cutting down on cigarettes and alcohol, and avoiding potential triggers such as stress and noise can help reduce the severity and regularity of migraines.
- Relaxation techniques, getting adequate sleep, and ensuring you stay hydrated are often recommended as part of a holistic approach to migraine management.
- Over-the-counter pain medications, such as ibuprofen or paracetamol, can help alleviate migraine pain in some cases.
Cluster headache treatment
Cluster headaches have specific treatments that are primarily focused on alleviating the intense pain during attacks (acute treatments) and preventing future occurrences where possible (preventive.)
A medication known as Verapmil is a popular course of preventative treatment for cluster headaches. However it has been shown to cause abnormal heart rhythms in some people, and requires regular heart (ECG) monitoring.
Triptans, usually sumatriptan, are sometimes effective in treating cluster headaches when administered as an injection or a nasal spray.
Pure oxygen, delivered through a mask for around 15-20 minutes, is another method employed to relieve the acute pain of cluster headaches.
Corticosteroids have been shown to be effective at providing short-term relief, however they aren’t recommended for long-term use and are often used as a temporary treatment until another is found.
Less common treatments for cluster headaches include:
- Electrical stimulation from a device known as a gammaCore, however this isn’t suitable for everyone.
- Greater Occipital Nerve (GON) block, a type of injection around the nerves at the back of the head. This has been shown to be on average 50% effective in treating cluster headaches, providing long-term relief.
- Lithium, melatonin, and a medical procedure known as Sphenopalatine Ganglion Stimulation can be effective, but aren’t commonly prescribed.
Painkillers such as paracetamol and ibuprofen are generally ineffective for cluster headaches.
The best way to identify the most effective treatment for you is to speak to your doctor. By discussing your condition with you, including potential triggers, severity, and regularity, they’ll be able to identify whether or not you’re experiencing cluster headaches, and what can be done.
Conclusion
In conclusion, migraines and cluster headaches, while both severe and debilitating in their own way, are quite different, and require different treatments to effectively manage.
Taking proactive steps to identify and better understand the condition you are experiencing is a vital part of finding the right course of action, allowing you to get back to living your life without fear of head pain.
References
https://www.ncbi.nlm.nih.gov/books/NBK544241
https://www.nhs.uk/conditions/cluster-headaches/
https://migrainetrust.org/understand-migraine/types-of-migraine/other-headache-disorders/cluster-headache
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5909131/
https://www.brainresearchuk.org.uk/neurological-conditions/cluster-headache





