What your vagina is trying to tell you
Written by Dr Gigi Taguri
The vagina can be a confusing and mysterious place. Many women confuse the vulva – the external female genitalia – with the internal muscular passage that is the vagina, and 65% have difficulty using the word ‘vagina’ itself.
As much as you try to ignore it, your vagina isn’t going anywhere, and by refusing to acknowledge what it’s up to you may be ignoring some pretty serious health warnings. To help you decode its messages, we’ve put together a list of common vaginal problems that you might want to watch out for.
Common vaginal problems
Knowing what is normal for you, such as your discharge and how this changes throughout your menstrual cycle, can make it easier to know what’s not normal. Spotting the signs of vaginal problems can help you get the treatment you need quickly and make any changes to help care for your genitals.
Here's a list of common problems in the genital area:
- Unusual discharge – this could be a change in colour, smell, or even texture (watch out for a favourite term among medical advisors: ‘cottage cheese’ vaginal discharge)
- Itchiness or soreness on the outside (the vulva)
- An internal itch (vaginal itch)
- Pain during sex
- Irregular bleeding – for example in between periods or after sex
- Lumps, blisters, and swelling on the vulva or anus
- Pain when urinating
These symptoms could be due to an STI or yeast infection.
Causes of vaginal infections
Vagninal and vulval infections can be caused by bacteria, fungus and viruses which can grow inside and around your vulva and vagina. Pain, itching and unsual discharge can be a sign of a vaginal infection, such as an STI or thrush.
Signs of an STI
Chlamydia
Chlamydia is spread though unprotected (without a condom) vaginal, anal or oral sex.
- Women chlamydia usually doesn’t cause any symptoms.
- Only a small percentage of people will notice a discharge or burning feeling when urinating.
That’s why it can be spread so easily- you simply don’t know you’ve got it. As one the most common STIs in the UK, it’s worth getting regularly tested for chlamydia.
Gonorrhoea
Also known as ‘the clap’, gonorrhoea is also caused by sex without condoms.
- Most women don’t notice anything because the infection usually starts inside you, in the cervix.
- Some women however notice irregular bleeding, lower tummy pain, a discharge or pain during sex or when urinating.
- Men usually notice a discharge from the penis or a burning sensation.
As with Chlamydia, this STI can be identified with the use of a test kit.
Trichomonas
Trichomonas (also known as “trich or TV) is more common than we once thought and testing for it is becoming more common. Like most STIs it’s passed on by sex without a condom or sharing sex toys. Most people do not know they have it, which is why it’s important to get regularly tested. Typical symptoms include:
- Itching
- Slightly fishy smelling thin greenish discharge
Herpes
Genital herpes usually comes and goes. It’s caused by the herpes virus (HSV). You’ll usually know that you have herpes because you will probably get all or some of these symptoms:
- a tingle or pain in the genital area, groin or lower back
- an itch, then redness that develops into blisters that will eventually pop and scab over
- After 2 weeks everything is back to normal
A herpes outbreak, particularly the first one, can be excruciatingly painful. Subsequent outbreaks are usually less severe. Some people get a discharge and depending on where the blisters are. It can be painful to pee.
Unfortunately, this STI can’t be ‘cured’ as such – only managed with treatments. Once you’ve got it, it will stay in your body for the rest of your life but the good news is that not everyone gets outbreaks. The virus can stay dormant in your body for a very long time or until you are run down or stressed.
Genital warts
Genital warts are caused by two low-risk strains of the human papillomavirus (HPV) Those low risk strains are not thought to be linked with cervical cancer. You can protect yourself against contracting them by getting an HPV vaccine.
- You may find clusters of small lumps around the opening of the vagina and around the vulva – they often have a cauliflower-like appearance and can feel slightly rough. They might itch, but they are usually not painful.
- Genital warts can also occur on the cervix, within the vagina, in and around the anus, and in the general groin area.
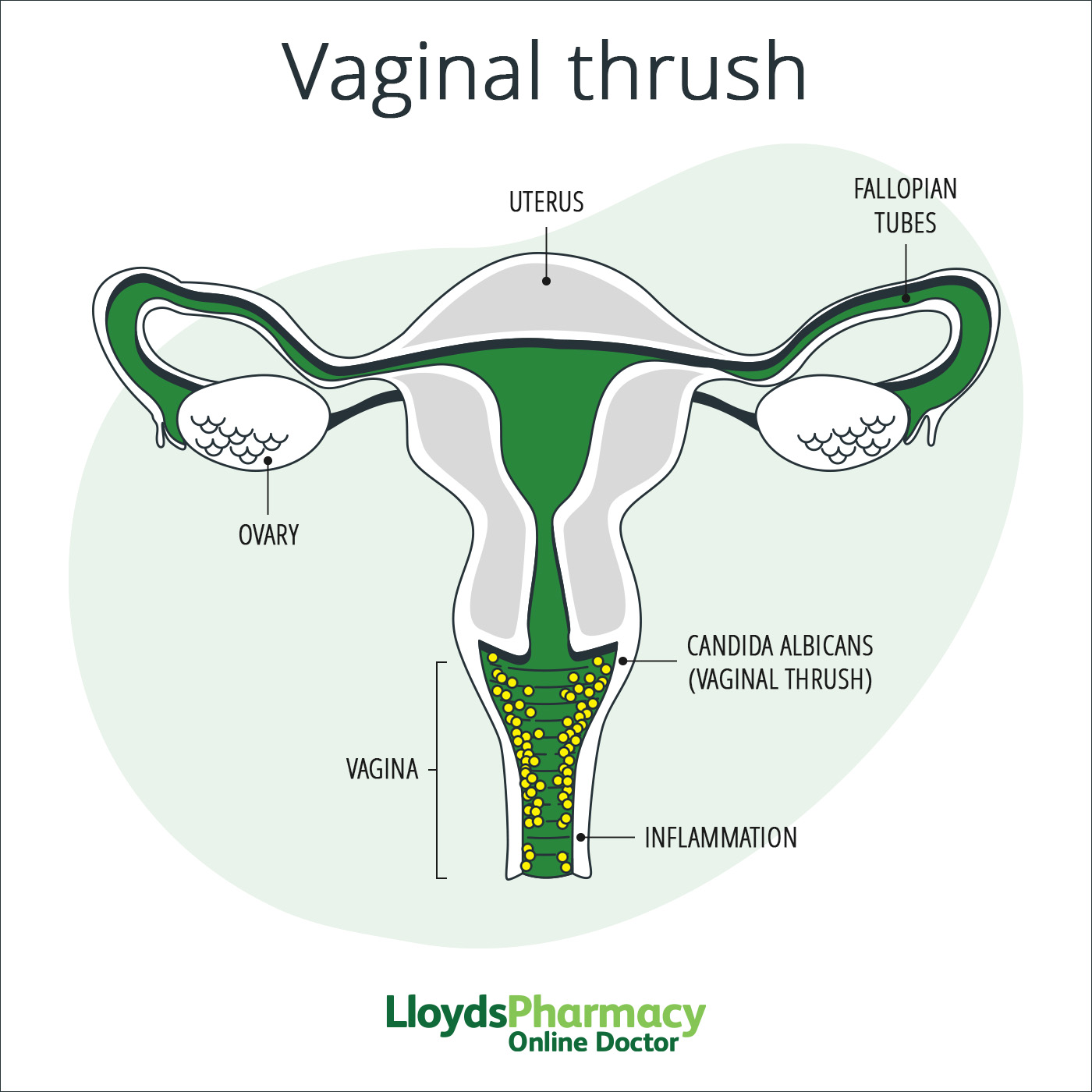
Signs of a yeast infection (thrush)
Similar to bacterial vaginosis, thrush can be the result of an imbalance. Thrush also known as vulvovaginal candidiasis is caused by a yeast called candida.
Don’t be alarmed – thrush is harmless, even though it can cause a lot of discomfort. Since most women will develop thrush at some point in their lives, it’s definitely worth knowing the symptoms.
What does vaginal thrush look like?
If you experience itching, burning, soreness or swelling around the vagina, or a lumpy, white, “cottage-cheese” like discharge, you probably have a bout of thrush. Luckily, it’s very simply treated with thrush tablets, creams or pessaries. Applying natural yoghurt can also help, but this can be a bit messy.
Signs of cystitis (UTI)
Cystitis is actually a urinary tract infection (UTI), but because one of the main symptoms (pain or burning when passing urine) can be confused with an STI.
You may have cystitis if you experience:
- a burning sensation when urinating
- an urge to pee more frequently
- finding it hard to hold on
This usually occurs when bacteria from the genital area or anus enter the urine tube (the urethra) and travel up into the bladder where they can multiply. That’s why drinking lots of fluids can help to flush out the bacteria. If untreated, the infection can spread further and cause a kidney infection.
Mild cystitis does not always require treatment and may clear up on its own.
If your cystitis persists you may need a course of antibiotics.
Signs of bacterial vaginosis (BV)
The vagina is full of different types of bacteria, keeping each other in check to create a certain, healthy environment. If this balance is disrupted the unhelpful bacteria can take over and cause so-called “bacterial vaginosis", BV for short.
This is not an STI, it’s an imbalance. It can be caused by over-washing or having a lot of sex without a condom because this can change the acid balance in your vagina - the pH.
Symptoms include:
- greyish/white discharge
- a fishy smell
You can do a simple self test that you can buy at your local pharmacy.
Other common vaginal and vulval problems
Aside from STIs, cystitis, thrush and BV, other common issues include:
Vulvitis
Sometimes irritation or soreness of the vulva (the external skin of your genitals) is not due to infection at all. Rather, it could be a reaction or hypersensitivity to substances such as soaps, bubble bath, shower gel, washing powder, lube, condoms or types of fabric.
Going “all natural” for a week or two should help ease the symptoms, but you can certainly soothe the area by applying your moisturiser or aloe vera gel (if you're not allergic).
It’s also worth mentioning that your vulva can also be affected by common skin conditions, including eczema and psoriasis, which can cause irritation and discomfort.
Folliculitis
This occurs when a hair follicle gets blocked and infected. It usually manifests itself as a series of red bumps or small spots around the vulva. Folliculitis in this region mainly occurs as a result of waxing, shaving, and wearing tight non-breathable fabrics.
Cases are usually mild and will clear of their own accord. Very occasionally, if the hair follicles become infected and you can see pus, you might need antibiotics.
How to maintain a healthy vagina
Looking after your vagina and vulva are really important. There are a few things you can do to promote a happy, healthy vagina.
- Don’t use water or soap inside your vagina (vaginal douching). Your vagina is actually pretty good at cleaning itself, and introducing irritating products can upset the complex bacterial interactions which keep your pH level just right. Washing the outside area with water and soap/shower gel is all you need to do. Trying to clean the inside passage could mean pushing bacteria higher up, potentially causing an infection or imbalance.
- Practice safe, clean sex. Always wear a condom with new sexual partners and make sure you wash any sex toys before and after use (it’s also very important you don’t share these with anyone else). It’s also a good idea to try and urinate after you’ve had sex, to flush out any bacteria around the urethra (urine pipe).
- Take STI tests regularly. This is particularly important if you have had several sexual partners or have ever had unprotected sex.
- Consider getting the HPV vaccine. Whilst protecting you against genital warts, this vaccine will also protect you against cervical cancer.
- Avoid wearing clothes that hold in heat and moisture. Leggings, tights and gym gear can create the perfect environment for yeast infections. Non-breathable tight fabrics such as nylon are prime culprits for this, so cotton underwear would be preferable.
- Avoid using strong detergents and soaps. Strongly perfumed bathing products and deodorants can cause irritation to your vaginal area. Also be conscious of the strength of the detergent you’re using to clean your underwear with.
- Be aware of side effects of prescribed antibiotics. Taking antibiotics can affect the balance of your vagina, increasing your chances of developing problems like thrush.
References
https://assets.publishing.service.gov.uk/NHS_Screening_Programmes_in_England_2017_to_2018_final.pdf
https://www.nhs.uk/conditions/gonorrhoea/symptoms/





